LGV is Chlamydia’s Wicked Stepsister. Don’t let the wicked stepsister ruin your fun.
LGV, Chlamydia’s Wicked Step Sister
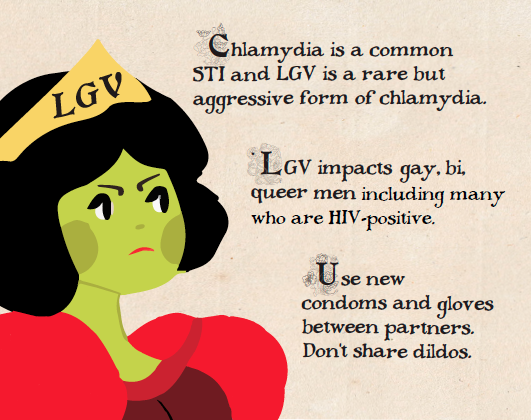
The common cold of sexually transmitted infections (STIs), chlamydia is one of most prevalent STIs in Canada. This is because its symptoms are relatively mild and can even, at times, go unnoticed.
Lymphogranuloma venereum, or just LGV, is an aggressive form of chlamydia. Unlike chlamydia, LGV symptoms are very noticeable and painful. Fortunately, LGV is also much more rare than regular chlamydia. It is usually well under 100 cases a year in a big city, relatively low when compared with other STIs.
However, LGV can be nasty and impact long term health if untreated. Recently, Toronto has seen a sharp increase in LGV exclusively among gay, bi, and queer men in Toronto, particularly among guys who are living with HIV.
Chlamydia can be treated easily with antibiotics. Treatment for LGV takes a little bit longer, but also involves antibiotics. The first step is getting tested. Left untreated, LGV can cause damage to sexual organs in both cis and trans men.
LGV Transmission
LGV can be transmitted by skin-to-skin contact of the mouth, cock, ass, front hole, or vagina with someone who has LGV. It can be spread by using the same glove, condom, sex toy, hand, or bare cock between multiple partners.
Infection with LGV occurs in three (3) stages.
STAGE 1:
3 days to 3 weeks after getting infected, a small, painless sore where the bacteria got into your mouth, cock, or inside your ass, front hole or vagina may appear. Many people don’t get a sore or don’t notice it. You will be able to give LGV to others from this point on.
STAGE 2:
10-30 days later, you might feel ill and have a fever and other flu like symptoms such as chills, joint pain, and decreased appetite.
STAGE 3:
Left untreated, LGV can progress and cause serious complications, years after the first infection. Hemorrhoid-like growths can appear, your genitals can swell painfully and the mucosal lining of your ass, front hole or vagina can become damaged. Left untreated LGV can cause damage to internal organs, scarring, and cause painful growths that require surgery to remove.
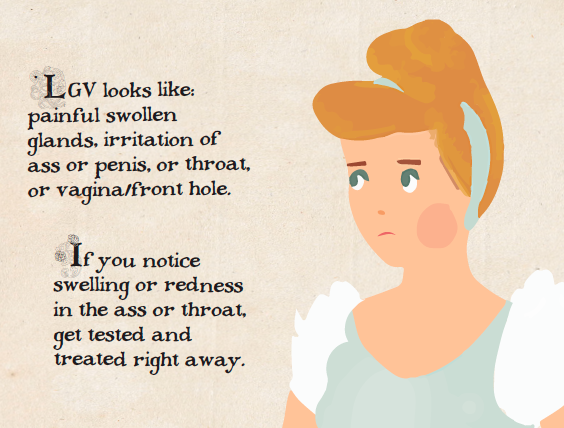
Other Symptoms
In addition to these 3 stages, you may experience other symptoms between or during these 3 stages. These may include the following:
- Inflammation and irritation (redness, swelling, throbbing sensation on the lining of your rectum, penis glans or urethra, front hole, vagina, or inside your mouth). You can transmit LGV with no symptoms.
- Shitting or peeing can feel urgent, constipated, painful or burn. You can develop painful ulcers in the ass. There can be blood or discharge from your genitals. It’s also possible to develop pus filled or bloody diarrhea.
Treating LGV
LGV is quickly cured with 3 weeks of antibiotics and leaves no lasting damage, so long as it’s caught early. Chlamydia is cured even faster, also with antibiotics.
Preventing LGV: Safer Sex
Condoms reduce the chances of getting LGV, as do gloves during fisting. Condoms and gloves should be changed between partners. Use separate sex toys for each person, or use a fresh condom each time it is inserted into a different partner.
Getting Tested for LGV
- Get tested right away if you have symptoms. Never ignore swelling.
- Get tested for Chlamydia and LGV once every 6 months if you have lots of sex partners.[i]
- Get tested once every 6 months to once per year if you only have a few sexual partners.
You will test positive for chlamydia if you have LGV. If a test comes back reactive for chlamydia but you also experience some of the more severe symptoms such as swollen glands and excessive swelling, ask your doctor about being tested specifically for LGV.
Always be clear with your doctor about which parts of your body you’re using when having sex. This is particularly important if they don’t know that you are having sex with other men. Testing for chlamydia and LGV involves swabbing the affected areas for samples of the bacteria. If whoever is doing the test assumes you’re a top and doesn’t swab your ass, a LGV infection could be missed.
For Poz Guys
LGV, like many STIs, makes it easier to pass on HIV if you have a detectable viral load.[iii] Treatment for HIV-positive guys is the same for HIV-negative guys, although some LGV treatment drugs can interact with some HIV medications.[iv]
- [i] Plus. Study: Regular use of PrEP May Reduce Bacterial Sexually Transmitted Infections. Feb 16, 2017. Retrieved Feb 16, 2017 from: http://www.hivplusmag.com/prevention/2017/2/16/study-regular-use-prep-may-reduce-bacterial-sexually-transmitted-infections
- [iii]Québec, Portal santé mieux-être. Lymphogranuloma Venereum (LGV). January 21, 2016.
- Retrieved Feb 2, 2017 from: http://sante.gouv.qc.ca/en/problemes-de-sante/lymphogranulomatose-venerienne-lgv/
- [iv] CATIE. Treatement Update 149. Key facts about LGV. April/May 2015. Retrived Feb 3, 2017 from: http://www.catie.ca/en/treatmentupdate/treatmentupdate-149/infection-fighters/key-facts-about-lgv
ACT is committed to the health and well-being of all gay men, regardless of their HIV status. We have a range of Group Programs for gay men that address issues related to depression, anxiety, substance use and body image, as well as programs for younger gay men that help them build resilience and community. We offer mental health counselling at ACT offices and in the community. Our staff are also trained to develop and deliver sexual health Outreach and Community Education programs.
As part of ACT’s Strategic Plan, Together Towards Zero, we are committed to leading in this area of healthcare because we have the experience, staff, and knowledge. Given our history and connection to the gay community in Toronto, we recognize the urgent need for leadership within this area, and are proud to be among those working towards building better supports for the different facets of our health.
Each year, ACT has produces resources that address issues pertaining to gay men’s health. Here’s what we have produced lately:
- Hep C and Sex for Gay Bi and Queer Guys
- Travelling with Prescribed Medication
- My Sex Life: info for young poz people
- BDSM: safer kinky sex
- Staying Off Crystal
One of ACT’s national partners has made these resources and others available to order. Find them at CATIE.ca
* We have chosen to use the term “gay” recognizing that this term may not resonate with all gay/bi/queer/2 Spirit men (including queer trans men). Our objective is simplicity of language and we recognize that our services and service networks must be equally skilled at being relevant and accessible to all men who have sex with men, regardless of how they understand their sexuality in relation to their core identity.